As of March 2021, cervical screenings for eligible individuals have fallen for the fourth consecutive year.
Overall in 2020-21, 70.2 per cent of eligible individuals aged between 25 and 64 had been screened within the required number of years. This signifies a two per cent decrease compared to 2019-20 when 72.2 per cent of eligible individuals were screened, according to data from NHS Digital.
Specifically in 2020-21 in the 25 to 49 age group, screenings of eligible individuals dropped to 68 per cent and in the 50 to 64 age group screenings dropped to 74.7 per cent.
Local authorities aim to have 80 per cent coverage which means 80 per cent of eligible individuals are screened within the required time frame. Out of the 149 local authority screening regions only 91 had reach a coverage of 70 per cent and no authorities reached the desired 80 per cent coverage.
Kensington and Chelsea in Greater London had the lowest coverage with 45.8 per cent and Derbyshire in the East Midlands had the highest coverage of 78.4 per cent in the 2020-21 period. In comparison Kingston upon Thames had an overall coverage of 64.8 per cent.
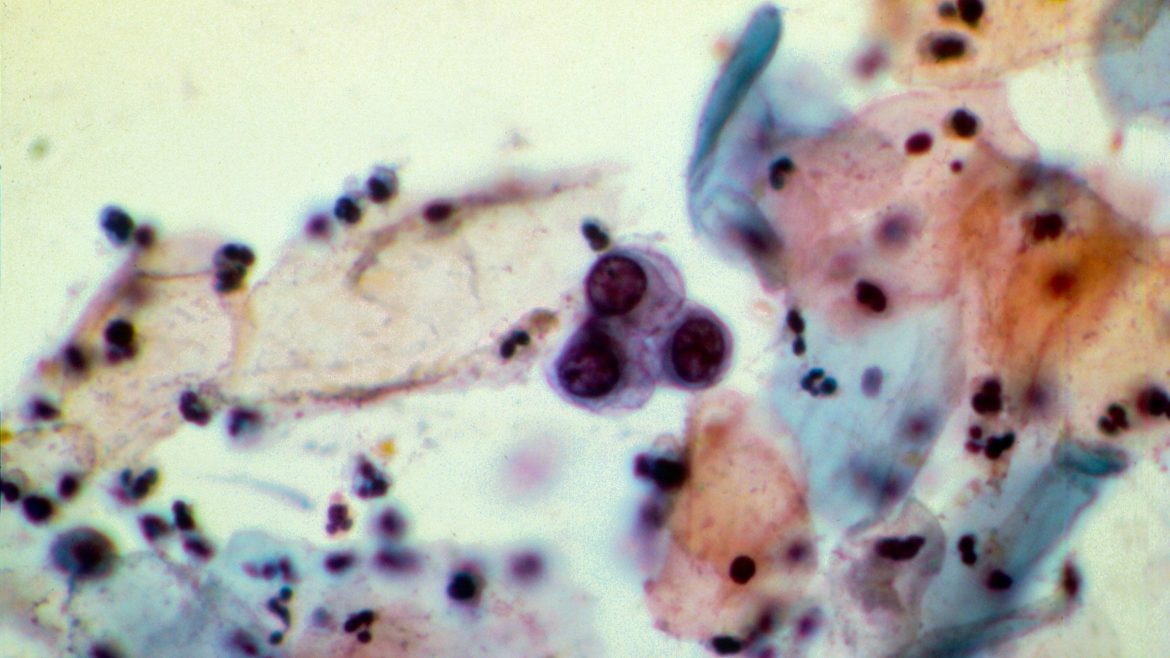
Cervical screenings (a smear test) are important as they are used to detect precancerous cells in the cervix which can be detected and removed before they develop into cancer.
The screenings test for a virus called human papilloma virus (HPV) which can cause cervical cells to become abnormal.
Eligible individuals are encouraged to attend their cervical screening and the test saves around 2,000 lives each year in the UK, according to Spire Healthcare.
The test involves a nurse or doctor collecting a small sample of cells lining the cervix to check if there are any changes.
Who can have a cervical screening?
Under the NHS Cervical Screening Programme eligible individuals are offered cervical screenings every three or five years depending on their age.
Those between the ages of 25 and 64 are invited for regular screenings under the programme. Individuals aged between 25 and 49 are invited for a screening every 3.5 years and those aged between 50 and 64 are invited for a screening every 5.5 years.
Why are people not booking screenings?
Estelle Keeber, 39, Instagram Expert and founder of Immortal Monkey has been on a mission to remind others to book their smear tests.
In November 2021, Keeber missed her smear test as she was grieving from her nan suddenly passing away and naturally having a smear test was the last thing on her mind.
When attending a GP appointment at a later date the receptionist picked up on her cancelled appointment and reminded her to rebook. Keeber took the first appointment they had.
She said: "At the time I was grieving and my own health was not a priority. As the weeks passed it did come to me to rebook but like many of us, I got distracted and never actually got around to it.”
Keeber said she thought that it was quite irresponsible to put off the test for so long, even unknowingly.
“I am fully aware of the risks and dangers and actually used having my smear test to encourage and remind others to book theirs,” she said.
Keeber shared a post on Instagram about her appointment in the hope just one other person would be reminded or triggered to book test. Later that day she had a response from someone thanking her for the reminder and telling her they had booked their smear test.
Tommy Powell, 25, an assessment and review officer in adult social care believes more could be done to support transgender people with cervical screenings.
“The reason people could be reluctant to have a cervical screening is because of the non-inclusive language used and people may feel unsafe to attend as they are worried about what will be said to them.”
Powell explained that as a transgender man, when he turned 25 he did not receive a letter from his GP inviting him for a screening.
“I didn’t get a letter because the GP had me down as male which is correct but I still have my cervix,” he said.
When he tried to book his appointment, he faced embarrassment at the GP’s and had to explain multiple times he had a cervix and was eligible for a screening.
“I had to explain to the receptionist that I was transgender and that I do have a cervix multiple times before I was allowed an appointment.”
Fortunately, Powell had a positive experience at his appointment and said: “When I eventually had my appointment, the nurse was lovely, she gave me a leaflet about being transgender and having a screening and that really did put me at ease.”
Powell is encouraging others to take up these vital screenings and said although it can be uncomfortable having the test can save lives.
“Obviously it wasn’t a pleasant experience but it was over and done with within two minutes. For me, two minutes of discomfort could save my life and that’s all that matters,” he said.
Information is available about screening programmes available to transgender and non-binary people and LGBT people.
What happens during a test?
The NHS has provided information for those attending screenings so they know what to expect.
The actual test takes around five minutes but the whole appointment can take around 10 minutes.
Patients will be asked to undress from the waist down behind a screen and will be given sheets to place over their body to protect their modesty.
A nurse or doctor will ask patients to lie back on a bed, usually with their legs bent, feet together and knees apart.
A smooth, tube-shaped tool (a speculum) is inserted into the vagina and the nurse or doctor uses the speculum and opens it so they can see into the cervix.
Using a soft brush a small sample of cells is taken from the cervix and the speculum is then removed. The patient can then get dressed and leave.
Results for the test usually arrive within two weeks.

Photo: Shutterstock
Saffron Watson, 26, a junior account executive, said she wanted others to share their experiences in the hope it normalises cervical screenings and people will not be so afraid of them and reluctant to book their test.
Watson determined to lead by example said: “I was determined that I was not going to be scared. I own my body, and I want to look after my health.”
She remembered receiving a letter from her GP six months before her 25th birthday and a few weeks later booked her appointment at the surgery. She was surprised that the screening was booked in as quickly as it was but looked forward to the experience and taking control of her body and health.
Watson suggests bringing a friend for support for those who might be nervous about attending: “A friend came with me to the doctors to keep me company, and it definitely helped to make it feel less scary and intimidating.”
When she booked her screening, she carried out some research and was sent an information leaflet with her letter which she found very helpful.
At the appointment Watson explained all she had to do was undress her lower half and sit in the stirrups and process of collecting her cervix samples was briefly uncomfortable but over very quickly and she had no pain or discomfort afterwards.
“My nurse was really friendly and asked me what I do, and even though it is just small talk it makes you feel a bit more relaxed,” she said.
She said the nurse who was collecting her sample was informative and explained to her that she could have some spotting afterwards and the results would be with her within two weeks.
Watson advices others to read up beforehand so they know what to expect: “You are the only one who knows your body and its capabilities. I figured that I might feel a bit of discomfort when the nurse uses the spreader (speculum) and takes a swab from inside your cervix. I prefer to read up and know what I'm walking into, even if it might be the worst outcome.”
The results can either be negative, have some abnormalities and on rare occasions if an “inadequate sample” is found the patient may be invited to be tested again or referred to colposcopy.
Watson received a negative test result two weeks later and is ready to book her next appointment when it is due.
She openly talks to her friends, many of whom are just over 25 and are eligible for screenings, about her experience to normalise the conversation.
Although she had her test done in March 2020 when the pandemic was starting, she believes Covid is no excuse for holding back on booking an appointment and urged anyone that still needs to book in to do so now.
“When you go in for the test, try your absolute best to relax - I know it is a hard thing to do, but it is going to hopefully make it more comfortable. Focus on something in the room and try to keep calm steady breaths, it should be over before you know it.”
Covid-19 disrupted screenings and attendance for screenings was less than usual in the early part of 2020-21. Those individuals considered to be at a higher risk of a significant cervical abnormality were prioritised for screenings during this period.
But even with Covid disruptions in 2020-21 only 4.59m individuals were invited for screenings which is a one per cent decrease to the previous year when 4.63m individuals were invited for screening.

Photo: Shutterstock
HPV Vaccine
Reality TV star Jade Goody died in 2009 aged 27 and was one of the most high-profile cervical cancer victims. Goody caused the “Jade Goody effect” and highlighted the dangers of cervical cancer to many young people.
Goody's family hope her story will inspire others to attend screenings and take up the HPV vaccine which was not available when Goody was at school.
After she died there was an extraordinary rise in eligible individuals attending cervical screenings. However, 10 years on numbers have dipped which could mean thousands of health concerns will not be picked up.
Girls and boys aged 12 to 13 years are offered the human papillomavirus (HPV) vaccine as part of the NHS vaccination programme.
The vaccine helps protect against cancers caused by HPV, including cervical cancer and some mouth and throat cancers.
For more information and support about going for cervical screening, results and treatment, you can contact Jo's Cervical Cancer Trust.