Lose weight, take the pill, don’t take the pill, eat healthy and come back to me when you want to have a child.
These are just some of the pieces of ‘advice’ women who suffer from Polycystic Ovary Syndrome (PCOS) hear and they say it is tiring.
PCOS is a hormonal disorder affecting one in ten women in the UK and is one of the most common endocrine disorders in women. But women with PCOS say that there is still not enough research into it.
PCOS can affect how the ovaries work and can lead to women having higher androgen levels (male hormones), more facial hair, insulin resistance, weight gain, hair loss, acne, irregular periods, and trouble getting pregnant.
Time and time again, women are given the same answers when they go and see their doctor about their symptoms.
“We’ll do a scan…. We’ll run some blood tests…”
“Yes, you have PCOS…. The best approach is to eat healthily and lose weight… We’ll put you on the pill…”
For women with PCOS the reality is not easy.
Mental Health
Researchers are yet to find a cure for this metabolic condition and that can make women feel lost, hopeless, and in need of an answer.
The contraceptive pill is one of the solutions that doctors prescribe to patients because it may help manage symptoms. However, the problem comes with a lack of information on the benefits and risks that come with the pill, leaving patients unsure about whether to take it or not.
For Natalie Hammers, 22, nurses had suggested that she take the birth control pill on top of other medication she was taking. She was sceptical about this and refused. The nurse had no other recommendations on what else she could do. A year later Hammers tried to get another opinion from an Obstetrician-Gynecologist where she was given the Ocella pill and had her IUD removed.
Doctors had also recommended that Hammers lose weight, leaving her frustrated. With weight loss being one of the main struggles that can come with PCOS, women can start to develop an eating disorder.
Hammers knows all too well how lack of guidance and comments on weight can lead to drastic solutions. She said: “I felt ignored and my concerns were pushed aside, like [the doctors] were irritated with me for having questions and wanting to find a solution.
“It seemed like they would not be willing to address my concerns until I lost weight. In a way, they are communicating that overweight people are not worthy of their time.”
The National Library of Medicine shows a study conducted in 2019 which investigated the relationship between women with PCOS and eating disorders, psychological distress, and self-esteem. They found that women with PCOS have a higher chance of developing an eating disorder due to psychological stress and low self-esteem.
Diagnosis for PCOS is often delayed until other health problems start to prop up. It is only until they start to develop other illnesses that it is taken seriously.
A study conducted on February 23, 2022, by BMC Women’s Health was conducted in Canada on patient satisfaction when it came to diagnosing women with PCOS.
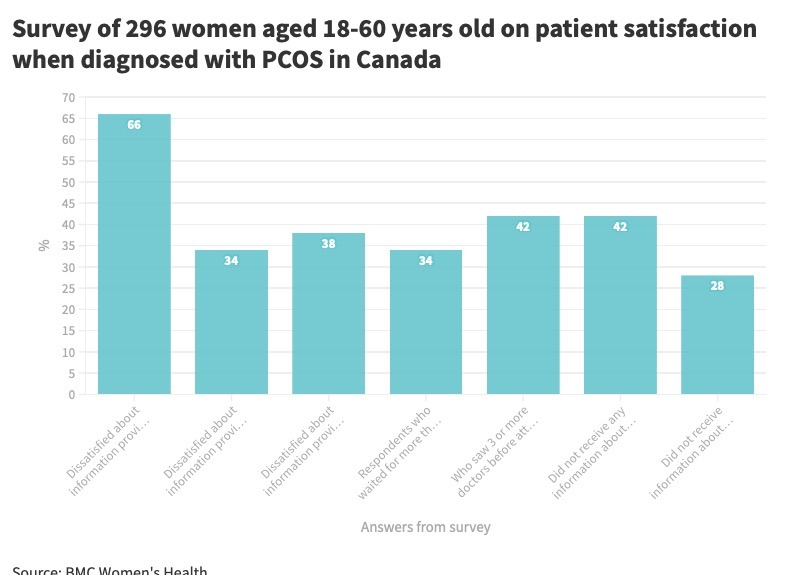
Patients found that there was no urgency when getting diagnosed with PCOS.
Binita Neupane, 28, said: “I gave up going to the doctors for advice because I was tired of hearing that there’s no cure.
“A little encouragement from the doctor would have made me feel a lot better. They don’t care unless you are trying to conceive. The main purpose should be to heal our body rather than just getting pregnant.”
Neupane resorted to doing her own research in hopes of finding the answers to questions that doctors simply could not.
Detaching stigmas from the pill
For some, the pill holds stigmas associated with sex and promiscuity which can go against their culture or family beliefs.
On International Women’s Day 2022, University of Birmingham had a talk hosted by Daisy PCOS, which is a research study that looks into the metabolic nature of PCOS. The talk involved discussions on the uses of the contraceptive pill and included a Q&A from women who were experiencing PCOS and who were still searching for answers.
Community and Public Engagement lead for Daisy PCOS Project Caroline Gillett, said: “It can be a little bit awkward… when the treatment option is the pill… and there is not really this understanding that it has other properties which are not contraceptive in nature which is important in terms of PCOS.
“The stigma attached to it being this contraceptive medication can be enough to make it awkward for young women. Depending on how conservative their parents are, they may feel that this isn’t the option for their child.”
Culture and religion have a big influence on how one can view medication which could potentially be beneficial for them. These associations can make people blind to the other issues attached to PCOS which are not to do with the ability to have children.
The PCOS Dr
Dr. Amina Hersi started her Instagram page @thepcosdr because she spent the past ten years not knowing about her PCOS. When she came across a very well-known Instagram page, she felt that it was very misinformed in the advice it was giving out.
She said: “I’m a doctor and I haven’t been taught a lot about PCOS, so I actually had to teach myself.”
Hersi said that during her training there was only one module on reproductive health. PCOS took up only half of a lecture and even then, it was about ovulation and infertility. It failed to go into detail about the long-term health impacts it could lead to such as heart disease, diabetes, and mental health problems.
Regarding the pill, Hersi said: “For me, who wasn’t trying to have kids at the time, it would have been so helpful to have extra help with my condition, so I think the pill has been vilified.
‘What I don’t like is social media guilt-tripping people who take the pill.”
She also said that people should give patients more information and explain both the benefits and risks that come with taking the pill.
“It should always be your own choice whether to take the pill or not.”
On March 14, 2022, Shadow Minister (Health and Social Care) Feryal Clark asked the Secretary for Health and Social Care whether a statement will be made by the department on the effects of PCOS and endometriosis on mental health.
With this, they had responded that: “Menstrual health and gynecological conditions, including endometriosis and PCOS, will be a priority within the forthcoming Women’s Health Strategy. We aim to publish the Strategy in spring 2022. We also plan to launch a public discussion paper later this year to inform the development of a new cross-Government mental health plan.”
So, is it about time we start reframing the way we think about PCOS or maybe change the name all together? The word ‘ovary’ in the name makes one think that this is only an issue that concerns women wanting to have children, but those who have the syndrome say it is much more than that.
For more information, you can visit the NHS website.





