No girls who received the human papillomavirus (HPV) vaccine when they were 12 or 13 have developed cervical cancer as women, a Scottish study published in January finds.
This is a significant finding as cervical cancer is the most common cancer in women under 35 in the UK.
There are over 100 types of HPV and most people will get it at some point in their lives, though only two high-risk strains cause the majority of HPV-related cancers.
The NHS advise it can be caught through any skin-to-skin contact of the genital area, vaginal, anal or oral sex, and through sharing sex toys.
While there is no treatment for the infection, most of the cancers caused by high-risk HPV variants can be prevented by vaccinating individuals before they become sexually active.
Scotland was the first of the four UK nations to start the vaccination programme in 2008.
Dr Tasmin Sommerfield, Clinical Advisor for Screening at National Screening Oversight (NSO), said:
“While the HPV vaccine protects against a lot of the different types of HPV virus that cause cancer, it can’t protect against them all so it’s still important that women go for regular cervical screening.
“Screening can find changes in the cells of your cervix even if you feel healthy and have no symptoms. If these are found at an early stage, they are much easier to treat.”
Kingston’s cervical cancer screening rate in women aged 25 to 49 during the last three and a half years is 63%, above the London average of 59% but still considerably below the mean for England of 68% and the target of 80%.
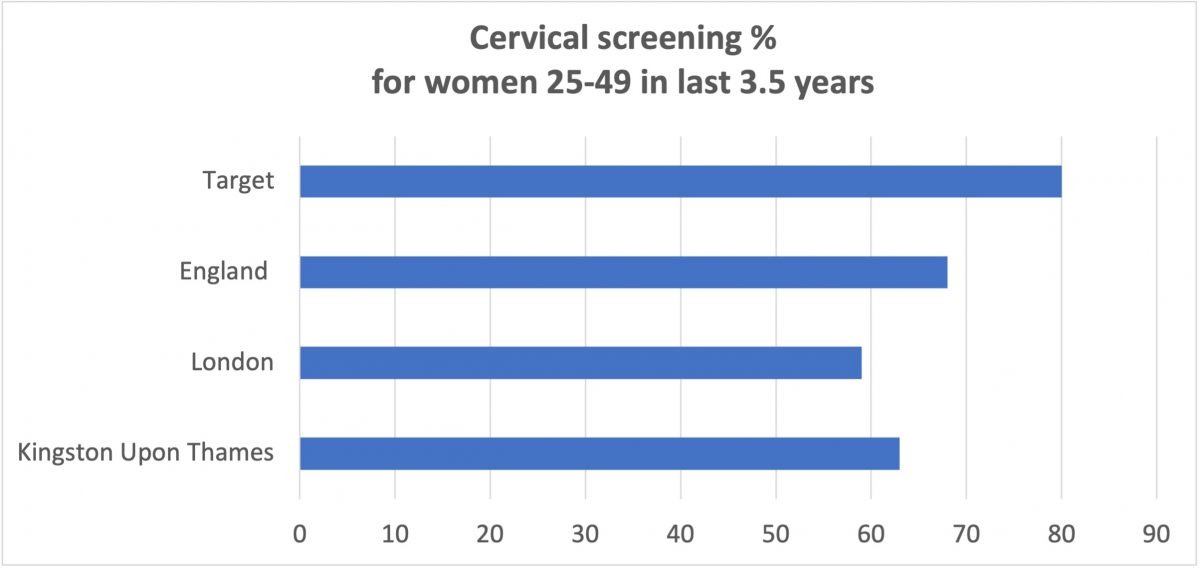
Screening take-up is vital to combatting the disease. It’s estimated 3791 women are diagnosed with cervical cancer in the UK every year, with over 1100 dying from it.
Dr Hossein Ashrafi, a professor of pathology and cancer biology at Kingston University, has led research over the past 16 years to demonstrate the link between HPV and various types of cancer in men and women.
Funded by Britain’s first e-money current account app dedicated to accelerating science and innovation, he is now leading research to develop a less harmful, lower-risk approach to treating cervical cancer.
The research will build on his team’s previous findings that showed how fig latex could inhibit HPV-induced cervical cancer by boosting tumour-suppressing proteins without harming healthy cells as current treatments do.
79% of invasive cervical cancers are attributed to HPVs 16 or 18 and 3.2% of women in the UK are estimated to have an HPV 16/17 infection at any given time.
Statistics from 2022/23 show that Kingston has well above average HPV vaccination rates for girls and boys in school, with Kingston achieving 11% more coverage for boys, than England as a whole.
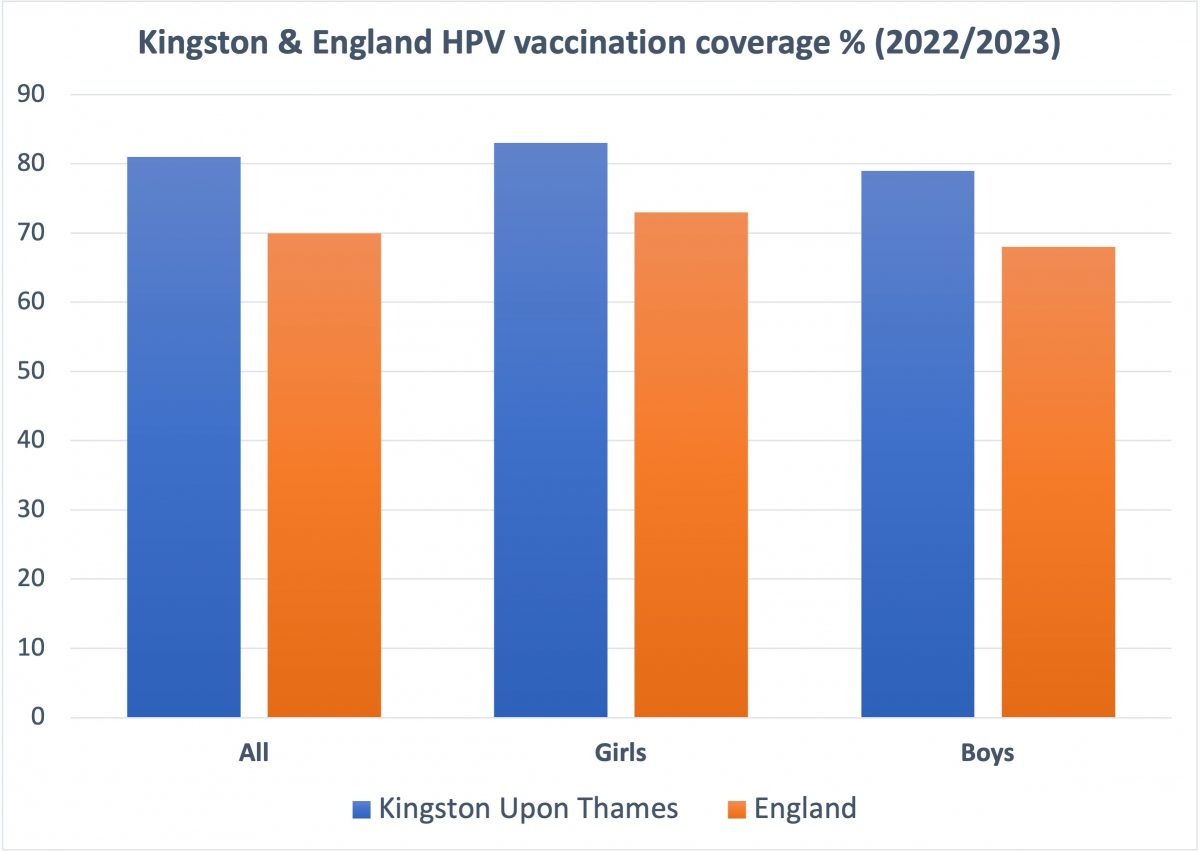
Kingston University’s Professor Giampiero Favato was pivotal in influencing the UK to extend the HPV vaccination programme to boys from September 2019.
His health economics research challenged the assumption that just vaccinating girls was more cost-effective and helped establish that the girls-only policy was inherently discriminatory.
The sexually transmitted infection can infect people of all genders and is a potential cause of penile cancer in men. It can also cause mouth, throat and anal cancer in both men and women, as well as other diseases.
Only vaccinating girls did not protect boys sufficiently and provided no protection at all for men who have sex with men.
The change in policy is expected to prevent more than 50,000 cases of cancer in men by 2058.
Favato’s research also influenced policy internationally and paved the way for gender-neutral vaccination programmes in many countries around the world.
In the UK, boys born after 1 September 2006 and girls under 25 who missed the vaccine at school are still eligible to get the vaccine and should contact their GP surgery.
Men under 45 who have sex with men, and other people at higher risk of HPV, are also eligible and should contact a sexual health clinic.
For those not eligible for the vaccine on the NHS, many pharmacies offer it for people up to 45 for a fee.
The vaccine also protects against genital warts.
Social infrastructure strategic planner, training for the NCTJ News Journalism qualification and publishing local news stories via the Kingston Courier.






