Kingston University’s healthcare partner has been ranked number one for research influence worldwide.
According to data from the Times Higher World University Rankings 2015-16, St George’s University Hospital is currently the best in the world at producing influential research.
Dr Henry Staines, a senior researcher at St George’s University Hospital, said: “The news was a very welcome surprise and really shows the strengths of smaller institutions such as ours.”
The university, based in Tooting, runs health and social care courses in partnership with Kingston University and shares its site with an NHS Trust.
Staines believes this “unique position” is responsible for the university’s rise up the rankings.
He said: “Sharing our site with the NHS Trust has encouraged collaborative studies, the results of which can often translate directly into the hospital and have a real impact on people’s health.
“In fact, we were rated fourth in the country for research impact when the government last rated the UK’s university network.”
Staines’ work at the Institute of Infection and Immunity has reinforced this ranking further.
Following his team’s latest research into malarial parasites, he is currently working closely with researchers worldwide to combat the recent Zika virus epidemic.
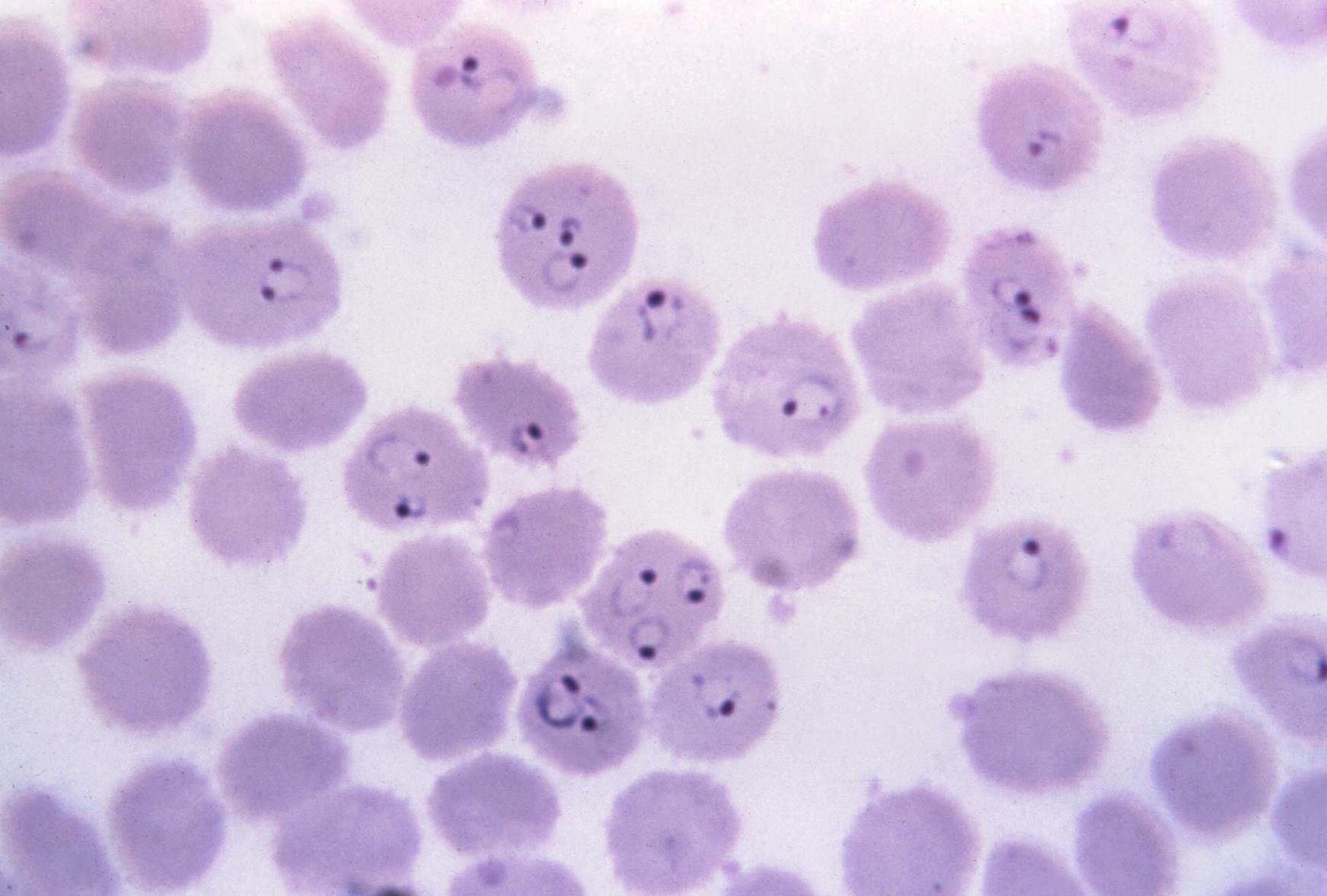
In a study published last week, Staines and his team of researchers exploited baker’s yeast to determine an important iron transport pathway used by malarial parasites, to survive within the human body.
Researchers altered the baker’s yeast DNA by removing a specific iron transport protein sequence from the yeast’s genome, similar to the sequence found in mosquito parasites.
“With the mutated yeast unable to make this iron transport protein, it loses the ability to grow when iron is present. We thought a protein from the malaria parasite might perform the same iron transporting role, as the one lacking in the mutant yeast,” Staines said.
Defining this iron transport pathway will now not only identify new ways to attack the parasite itself but will also help to understand how our current anti-malarial drugs work, according to Staines.
He added: “This knowledge is important because antimalarial drugs such as artemisinin-based combination therapies are not as effective as they used to be in South East Asia, which is a worrying trend.”
Staines is currently working on developing the next generation point-of-care diagnostics for malaria, together with the medical device company QuantuMDx.
“Their hand-held, battery-operated devices can give a diagnosis from a drop of blood in under 15 minutes,” he said.
“By identifying specific sequences of DNA, their technology will not only be able to tell if you have malaria but will also tell you which species of malarial parasite is causing your disease and indicate the correct choice of drug to use against it.
“This would offer personalised medicine in resource-poor settings where malaria is still rampant.”
The technology can also be used to diagnose diseases other than malaria.
Staines continued: “This is a platform technology being used to develop diagnostics for other established infectious diseases such as tuberculosis and sexually transmitted diseases.
“For example, we recently started a project to detect dengue virus. This became timely when the Zika virus outbreak hit the news, as we are now in an excellent position to respond to this emerging threat.
“Both dengue and Zika are closely related viruses, are transmitted by the same mosquitoes, and have similar initial symptoms, so being able to distinguish between them quickly would make an important difference to patient management.”